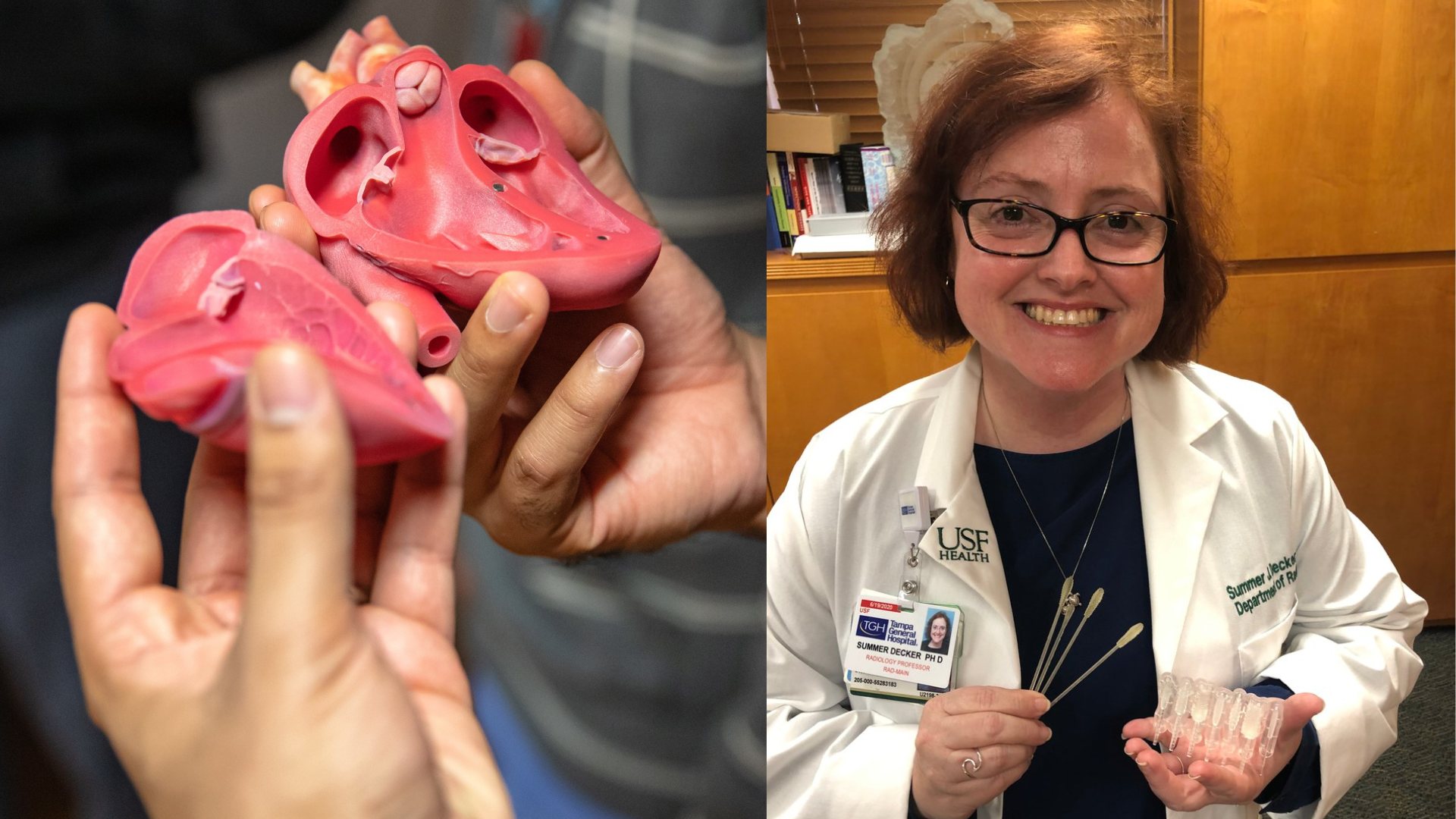
How do you mend a broken heart? With plastic. That’s a goal at Tampa General Hospital, where a sophisticated 3D printing program is making replicas of human organs from layers of artificial materials. Teaming up with the USF Health Morsani College of Medicine’s Department of Radiology, Tampa General has used 3D printing for planning aortic valve replacements, trauma surgery, cancer surgery and other reconstructions, as well as creating replicas of major organs. The replicas are used by surgeons to improve planning for surgery with the goal of a better surgical experience and outcomes for the patient.
“We’re able to translate medical imaging data into 3D models and these can be used in clinical decision-making, medical simulation and training, as well as patient education,” said Summer Decker, PhD, professor and director of 3D Clinical Applications for the Department of Radiology at the USF Health Morsani College of Medicine.
This potentially revolutionary technique uses 3D-printed facsimiles to better understand treatment and even reduce risk in invasive and complex surgeries. It allows for an appraisal of an organ outside the body, which saves time in the operating room and reduces costs. “Because of this 3D technology, we can take an 11-hour surgery down to a three-hour surgery,” Decker added. “So, it makes for safer and more efficient procedures.”
The USF Health Morsani College of Medicine and Tampa General are the first in the Tampa Bay area and among the first in the country to utilize this innovative technology. Although this collaborative 3D printing program started as research years ago, it has advanced to become a valued medical asset today. Early in the COVID-19 pandemic, for instance, Dr. Charles Lockwood, senior vice president of USF Health and dean of the Morsani College of Medicine, asked the USF Health 3D lab team to develop a solution for the international supply shortage for the nasal swabs needed for COVID-19 testing. Working in collaboration with USF’s Division of Infectious Disease and Tampa General’s Global Emerging Diseases Institute, the team designed and developed a 3D-printed alternative nasopharyngeal swab for COVID testing. Validating the accuracy of the swab took place in several health care facilities across the U.S., including Tampa General Hospital. To date, the USF patent-pending design has produced more than 75 million swabs in over 50 countries.
A swab is one thing; a heart is another. The artificial version gives physicians and patients a better understanding of the problem at hand. So, if a patient has a bad heart, doctors can scan it, print it, and collaborate on a strategy based on the printed model. Just as important, they can put it in the patient’s hands. “It gives our patients and doctors a better understanding of the problem and how best to treat it,” said Dr. Krishna Nallamshetty, chair of the Department of Radiology and associate professor of Radiology and Cardiology at the USF Health Morsani College of Medicine and chief of staff at Tampa General Hospital.
A 3D-printed anatomical model or surgical cutting guide is made with using different types of medical imaging such as computed tomography (CT) or magnetic resonance imaging (MRI) scans. Then, a 3D printer makes a copy of the object through a series of compiled layers. This “additive manufacturing” process lays down extremely thin layers of material in a liquid form and fuses them together to create a replica of the digital file. The technique can make complex shapes and sizes with a minimum of materials, so it’s fast and relatively inexpensive.
“It’s true bench to bedside in a short time frame, often same day,” Decker said. “We can scan the patient, make a computer model of the organ or design a surgical cutting guide, use it to collaborate with all the teams so they know exactly what they need, print it, and then scrub it for surgery. It’s an innovation that helps change the outcome for the patient.”
“Having an exact replica of a patient’s real heart – including defects – is an invaluable tool, especially when it can be created in less than a day,” said Jonathan Ford, PhD, assistant professor and biomedical engineer, Department of Radiology, USF Health Morsani College of Medicine and the technical director for 3D printing, Tampa General Hospital. “A heart will take about 15 hours to reproduce on the printer, so by the time we come back in the morning, we can hand off the printed heart to the surgeon for reference.”
The 3D clinical applications team currently houses seven medical grade 3D printers. The team has been located at the USF Health South Tampa Center for Advanced Healthcare on the Tampa General campus for the past eight years. The team plans to relocate their 3D lab and printers inside the main hospital radiology department, providing better access for surgeons and other clinicians at Tampa General.
Decker and USF Health’s 3D clinical applications team were also recognized for their work on the 3D-printed nasal swabs with the inaugural Jack A. Kolosky Award for Healthcare Innovation from the Tampa Innovation Partners in 2021. The Kolosky Award is named after the retired president of Moffitt Cancer Center and recognizes health care innovation.
In addition, for her pioneering work with the 3D-printed swab, Decker was among three USF Health faculty members in June 2021 to share the national spotlight with health care professionals from across the country – including Chief Medical Advisor to the President of the United States, Dr. Anthony Fauci – for being named 2021 Champions of Humanistic Care by the Arnold P. Gold Foundation.
“This is really about the power of collaboration between USF and Tampa General because the work being done here is truly transformational,” said John Couris, president and CEO of Tampa General Hospital. “It’s making a huge difference to our physicians and to our patients.”
TAMPA GENERAL HOSPITAL: www.tgh.org
USF HEALTH: health.usf.edu


